SATA Questions for NCLEX-RN with Answers and Rationales
A nurse is caring for a client with heart failure. Which of the following interventions should the nurse include in the plan of care? (Select all that apply)
A. Monitor daily weights
B. Encourage a high sodium diet
C. Administer diuretics as prescribed
D. Teach the client to recognize signs of fluid overload
E. Limit fluid intake as appropriate
Correct Answers: A, C, D, E
Rationale: Daily weights help monitor fluid retention, diuretics help reduce fluid overload, educating about fluid overload signs is essential, and fluid intake should be limited as needed to prevent exacerbation of heart failure.
A nurse is assessing a client with diabetes mellitus. Which findings should the nurse document as potential complications? (Select all that apply)
A. Foot deformities
B. Visual changes
C. Increased thirst
D. Frequent infections
E. Weight gain
Correct Answers: A, B, C, D
Rationale: Foot deformities, visual changes, increased thirst, and frequent infections can all be complications of poorly managed diabetes mellitus.
The nurse is preparing to administer antibiotics to a client with a severe infection. Which considerations are essential? (Select all that apply)
A. Assess for allergies to medications
B. Obtain cultures before starting therapy
C. Administer all doses at the same time of day
D. Monitor for signs of superinfection
E. Teach the client to stop taking the medication when symptoms improve
Correct Answers: A, B, D
Rationale: Assessing allergies is crucial to prevent adverse reactions; cultures should be obtained before starting antibiotics to ensure appropriate treatment; monitoring for superinfections is critical when patients are on antibiotics.
A nurse is teaching a group of students about infection control. Which practices should the nurse emphasize? (Select all that apply)
A. Hand hygiene before patient contact
B. Using gloves for all patient interactions
C. Disposing of sharps in a designated container
D. Performing sterile dressing changes only in the operating room
E. Wearing masks in isolation rooms
Correct Answers: A, C, E
Rationale: Hand hygiene is vital in infection control, proper disposal of sharps prevents needlestick injuries, and wearing masks in isolation rooms is important for infection prevention.
The nurse is conducting discharge planning for a client with asthma. Which instructions should be included? (Select all that apply)
A. Recognize and avoid triggers
B. Use the rescue inhaler prior to exercise
C. Monitor peak flow daily
D. Keep a log of symptoms and medication use
E. Discontinue medications if well-controlled
Correct Answers: A, B, C, D
Rationale: Avoiding triggers, using rescue inhalers, monitoring peak flow, and logging symptoms are all key components in managing asthma.
A nurse is caring for a postpartum client who had a cesarean section. Which findings should prompt immediate nursing actions? (Select all that apply)
A. Severe abdominal pain
B. Foul-smelling lochia
C. Elevated temperature
D. Urinary retention
E. Breast tenderness
Correct Answers: A, B, C, D
Rationale: Severe abdominal pain may indicate complications, foul-smelling lochia suggests infection, elevated temperature may signal infection, and urinary retention can indicate complications from anesthesia.
A nurse is preparing to administer an anticoagulant to a patient. Which nursing actions are necessary? (Select all that apply)
A. Assess the patient’s blood pressure
B. Monitor for signs of bleeding
C. Administer using a large bore needle
D. Educate the patient on dietary restrictions
E. Check the patient’s INR if applicable
Correct Answers: A, B, D, E
Rationale: Assessing blood pressure is necessary, monitoring for bleeding is critical after anticoagulant administration, dietary restrictions aim to ensure safety, and INR checks are necessary to monitor anticoagulation status.
A nurse is educating a client with chronic obstructive pulmonary disease (COPD) about self-management. Which statements by the client indicate a need for further teaching? (Select all that apply)
A. “I can continue smoking as long as I take my medications.”
B. “I should get my flu shot every year.”
C. “I’ll use my inhaler only when I feel short of breath.”
D. “I need to stay hydrated to help with my breathing.”
E. “I’ll use supplemental oxygen during my activities.”
Correct Answers: A, C
Rationale: Smoking cessation is crucial for COPD management, as is understanding when to use inhalers. The option regarding only using inhalers when symptomatic indicates misunderstanding.
The nurse is caring for a client with a spinal cord injury at C6. Which self-care deficits should the nurse anticipate? (Select all that apply)
A. Dressing independently
B. Bowel and bladder control
C. Mobility in upper extremities
D. Personal hygiene
E. Eating independently
Correct Answers: A, B, D
Rationale: A C6 injury primarily affects upper extremity control, impacting dressing, bowel, and bladder control; personal hygiene may also be challenging.
A nurse is discussing dietary modifications with a client newly diagnosed with hypertension. Which recommendations should the nurse make? (Select all that apply)
A. Increase potassium intake
B. Limit saturated fat
C. Reduce sodium
D. Drink alcohol in moderation
E. Eat more processed foods
Correct Answers: A, B, C, D
Rationale: Dietary recommendations include increasing potassium, limiting saturated fats, reducing sodium, and drinking alcohol in moderation to manage hypertension.
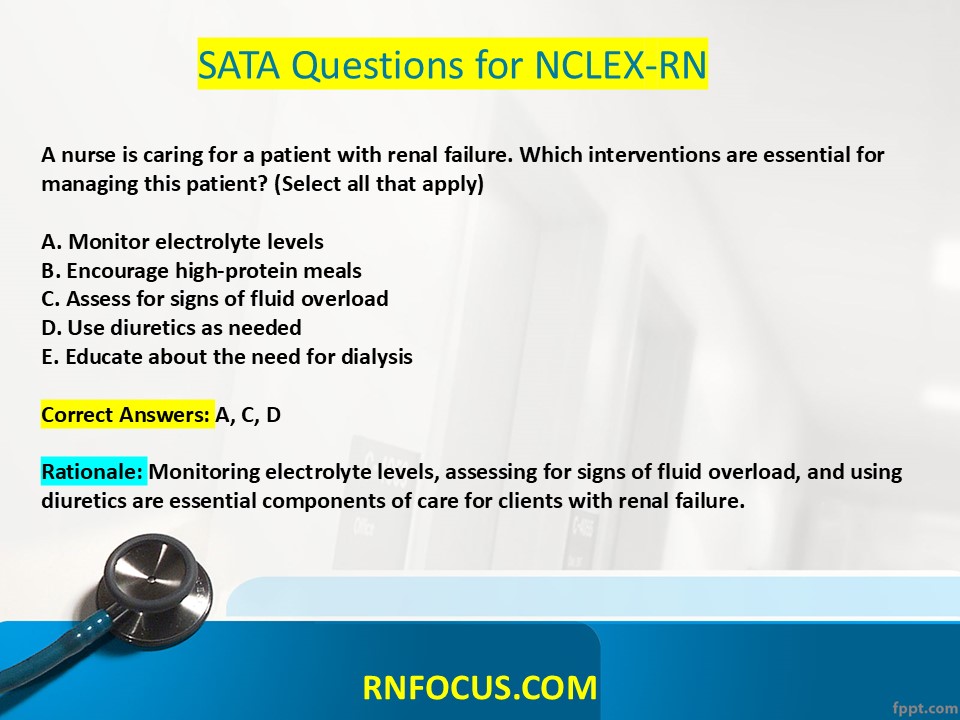
A nurse is caring for a patient with renal failure. Which interventions are essential for managing this patient? (Select all that apply)
A. Monitor electrolyte levels
B. Encourage high-protein meals
C. Assess for signs of fluid overload
D. Use diuretics as needed
E. Educate about the need for dialysis
Correct Answers: A, C, D
Rationale: Monitoring electrolyte levels, assessing for signs of fluid overload, and using diuretics are essential components of care for clients with renal failure.
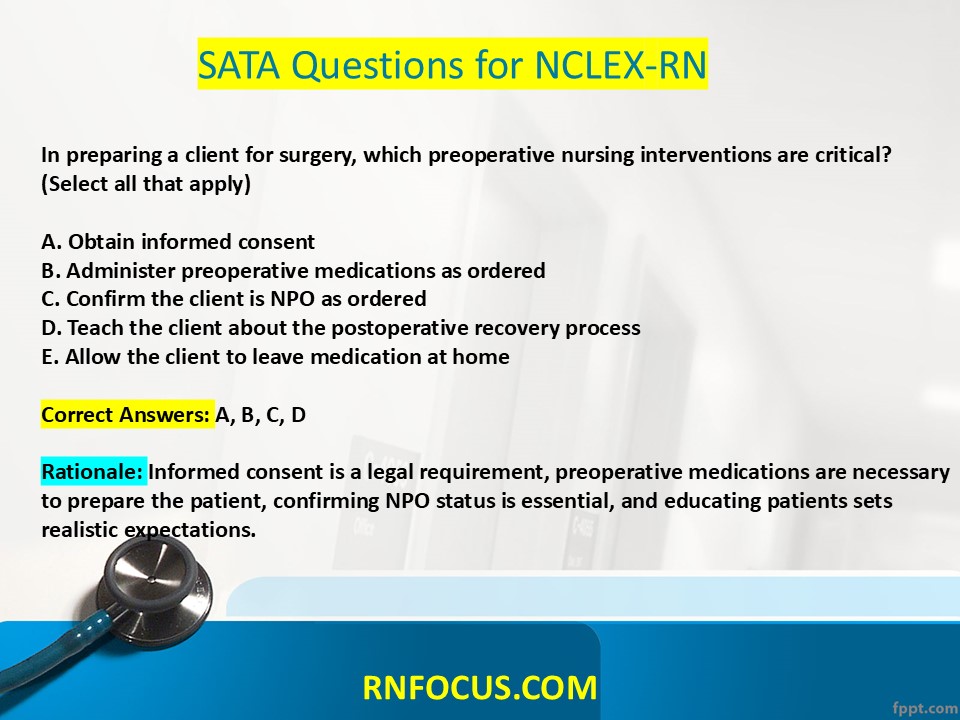
In preparing a client for surgery, which preoperative nursing interventions are critical? (Select all that apply)
A. Obtain informed consent
B. Administer preoperative medications as ordered
C. Confirm the client is NPO as ordered
D. Teach the client about the postoperative recovery process
E. Allow the client to leave medication at home
Correct Answers: A, B, C, D
Rationale: Informed consent is a legal requirement, preoperative medications are necessary to prepare the patient, confirming NPO status is essential, and educating patients sets realistic expectations.
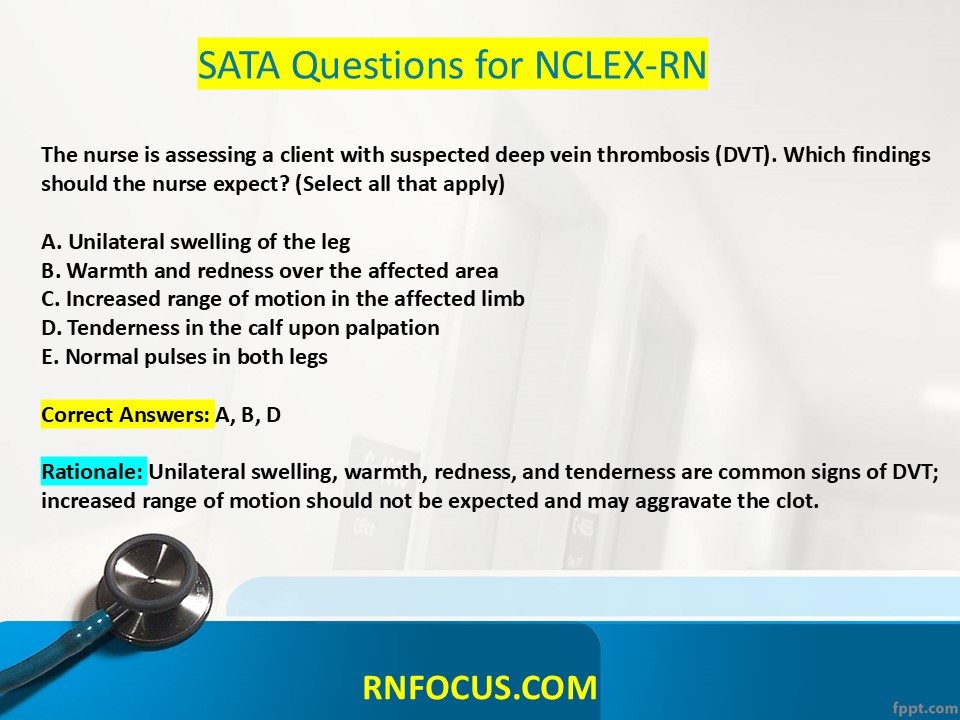
The nurse is assessing a client with suspected deep vein thrombosis (DVT). Which findings should the nurse expect? (Select all that apply)
A. Unilateral swelling of the leg
B. Warmth and redness over the affected area
C. Increased range of motion in the affected limb
D. Tenderness in the calf upon palpation
E. Normal pulses in both legs
Correct Answers: A, B, D
Rationale: Unilateral swelling, warmth, redness, and tenderness are common signs of DVT; increased range of motion should not be expected and may aggravate the clot.
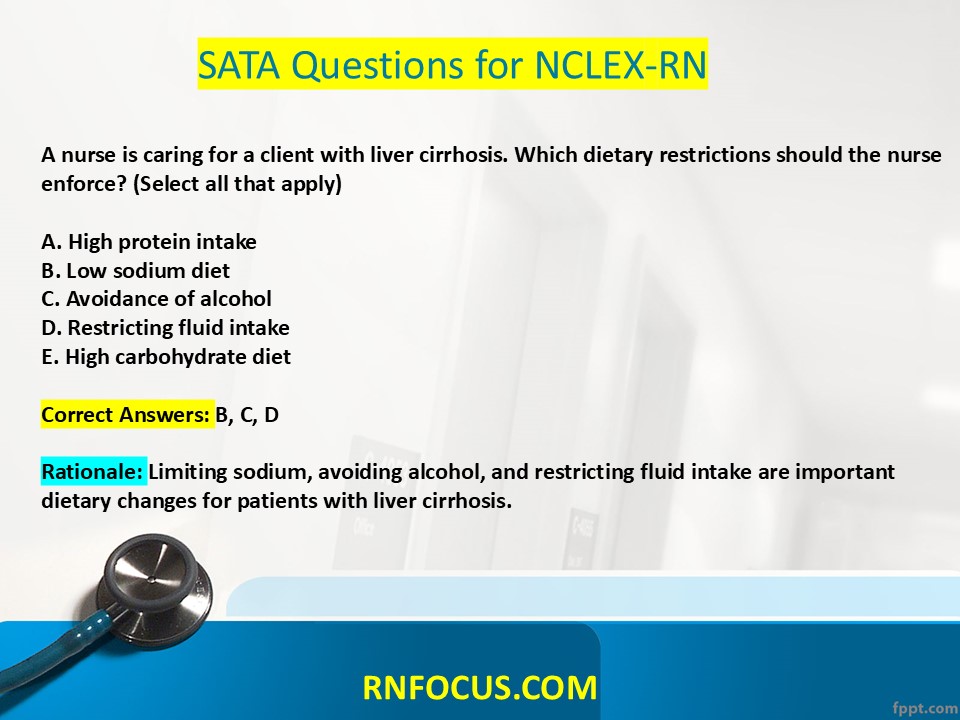
A nurse is caring for a client with liver cirrhosis. Which dietary restrictions should the nurse enforce? (Select all that apply)
A. High protein intake
B. Low sodium diet
C. Avoidance of alcohol
D. Restricting fluid intake
E. High carbohydrate diet
Correct Answers: B, C, D
Rationale: Limiting sodium, avoiding alcohol, and restricting fluid intake are important dietary changes for patients with liver cirrhosis.
The nurse is assessing a child with possible meningitis. Which signs and symptoms should the nurse monitor for? (Select all that apply)
A. Nuchal rigidity
B. Photophobia
C. Rash
D. Lethargy
E. High fever
Correct Answers: A, B, D, E
Rationale: Nuchal rigidity, photophobia, lethargy, and high fever are classic signs of meningitis.
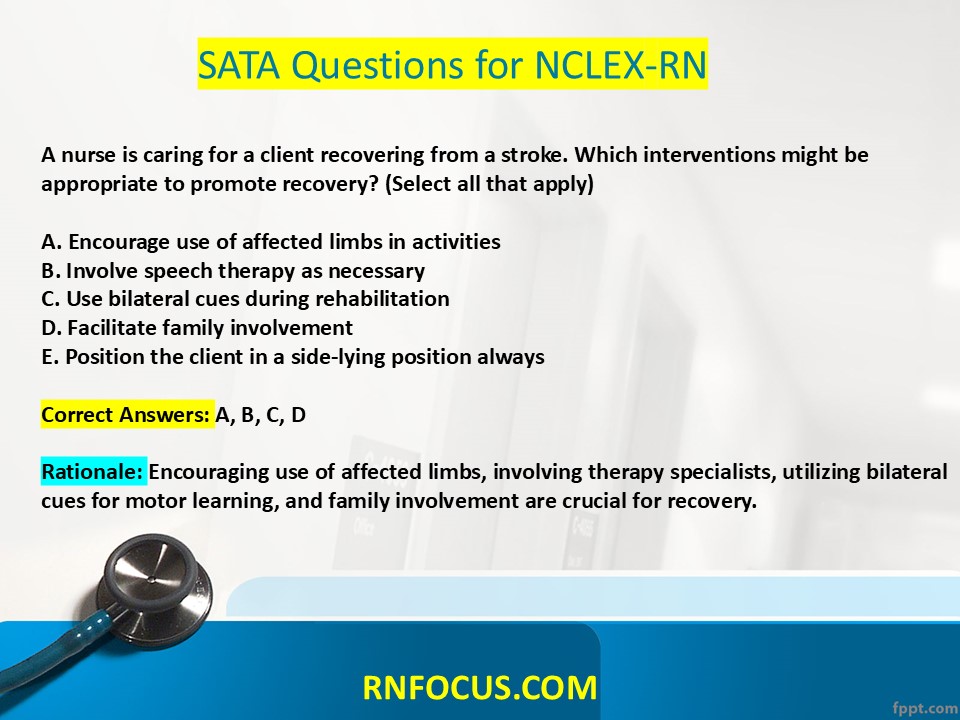
A nurse is caring for a client recovering from a stroke. Which interventions might be appropriate to promote recovery? (Select all that apply)
A. Encourage use of affected limbs in activities
B. Involve speech therapy as necessary
C. Use bilateral cues during rehabilitation
D. Facilitate family involvement
E. Position the client in a side-lying position always
Correct Answers: A, B, C, D
Rationale: Encouraging use of affected limbs, involving therapy specialists, utilizing bilateral cues for motor learning, and family involvement are crucial for recovery.
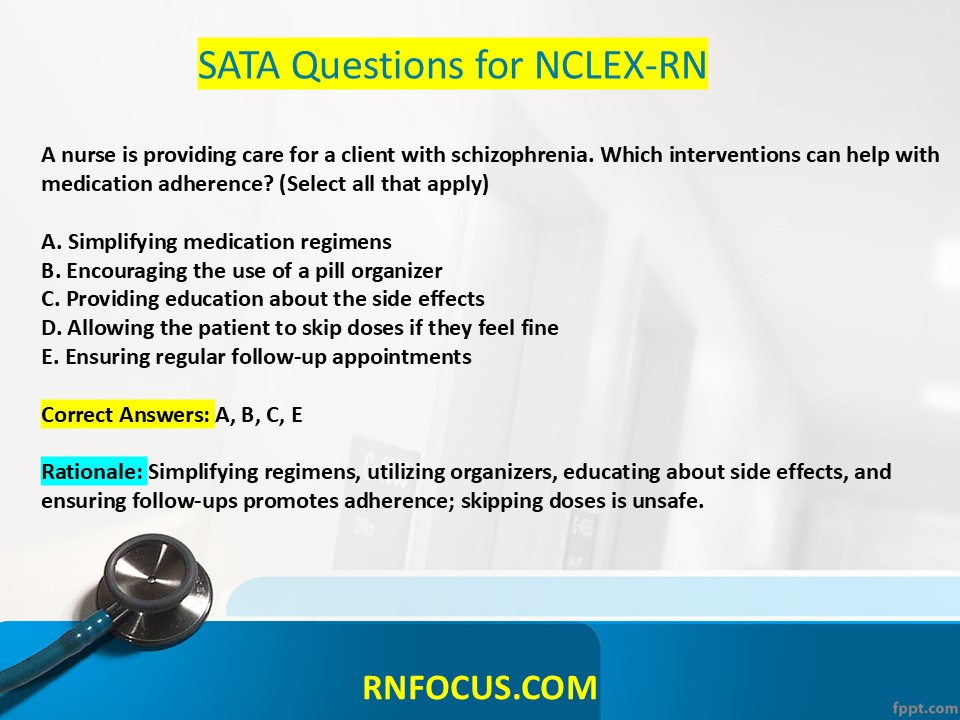
A nurse is providing care for a client with schizophrenia. Which interventions can help with medication adherence? (Select all that apply)
A. Simplifying medication regimens
B. Encouraging the use of a pill organizer
C. Providing education about the side effects
D. Allowing the patient to skip doses if they feel fine
E. Ensuring regular follow-up appointments
Correct Answers: A, B, C, E
Rationale: Simplifying regimens, utilizing organizers, educating about side effects, and ensuring follow-ups promotes adherence; skipping doses is unsafe.
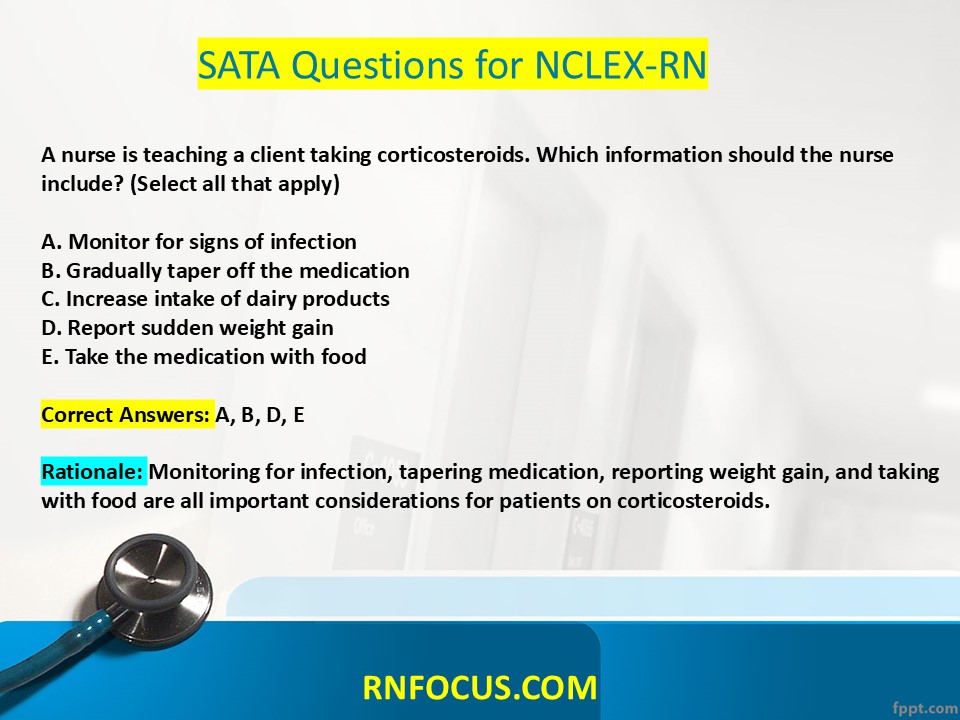
A nurse is teaching a client taking corticosteroids. Which information should the nurse include? (Select all that apply)
A. Monitor for signs of infection
B. Gradually taper off the medication
C. Increase intake of dairy products
D. Report sudden weight gain
E. Take the medication with food
Correct Answers: A, B, D, E
Rationale: Monitoring for infection, tapering medication, reporting weight gain, and taking with food are all important considerations for patients on corticosteroids.
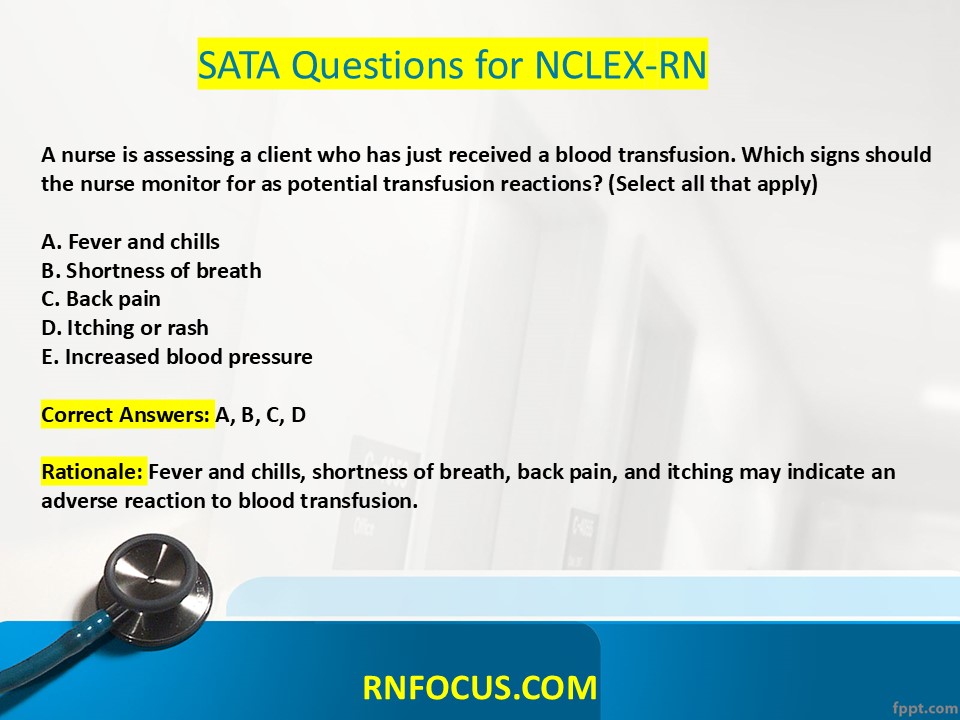
A nurse is assessing a client who has just received a blood transfusion. Which signs should the nurse monitor for as potential transfusion reactions? (Select all that apply)
A. Fever and chills
B. Shortness of breath
C. Back pain
D. Itching or rash
E. Increased blood pressure
Correct Answers: A, B, C, D
Rationale: Fever and chills, shortness of breath, back pain, and itching may indicate an adverse reaction to blood transfusion.
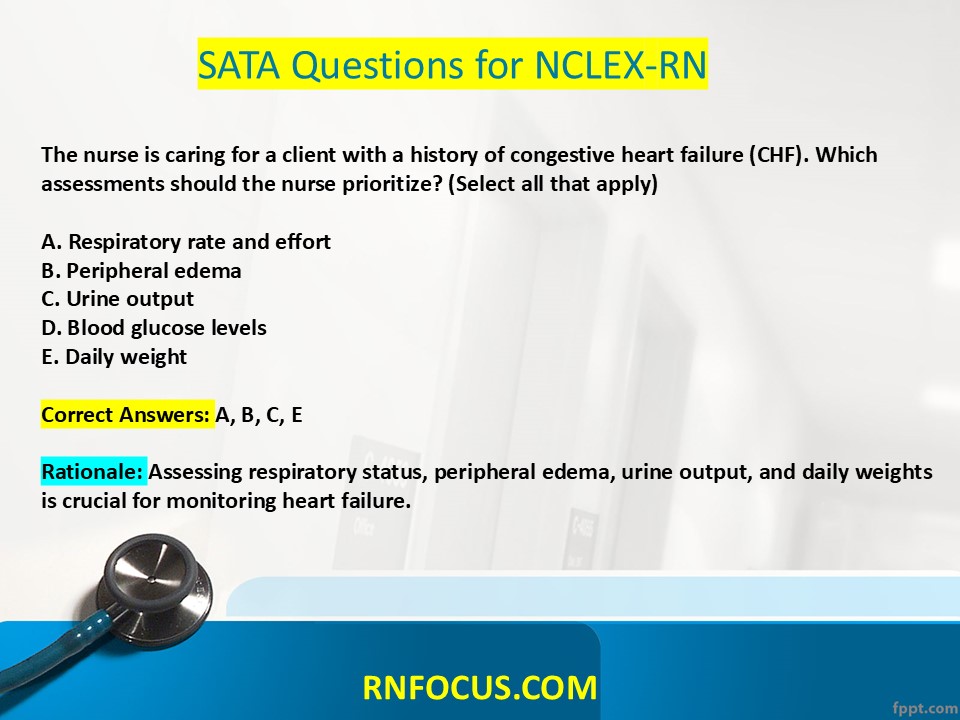
The nurse is caring for a client with a history of congestive heart failure (CHF). Which assessments should the nurse prioritize? (Select all that apply)
A. Respiratory rate and effort
B. Peripheral edema
C. Urine output
D. Blood glucose levels
E. Daily weight
Correct Answers: A, B, C, E
Rationale: Assessing respiratory status, peripheral edema, urine output, and daily weights is crucial for monitoring heart failure.
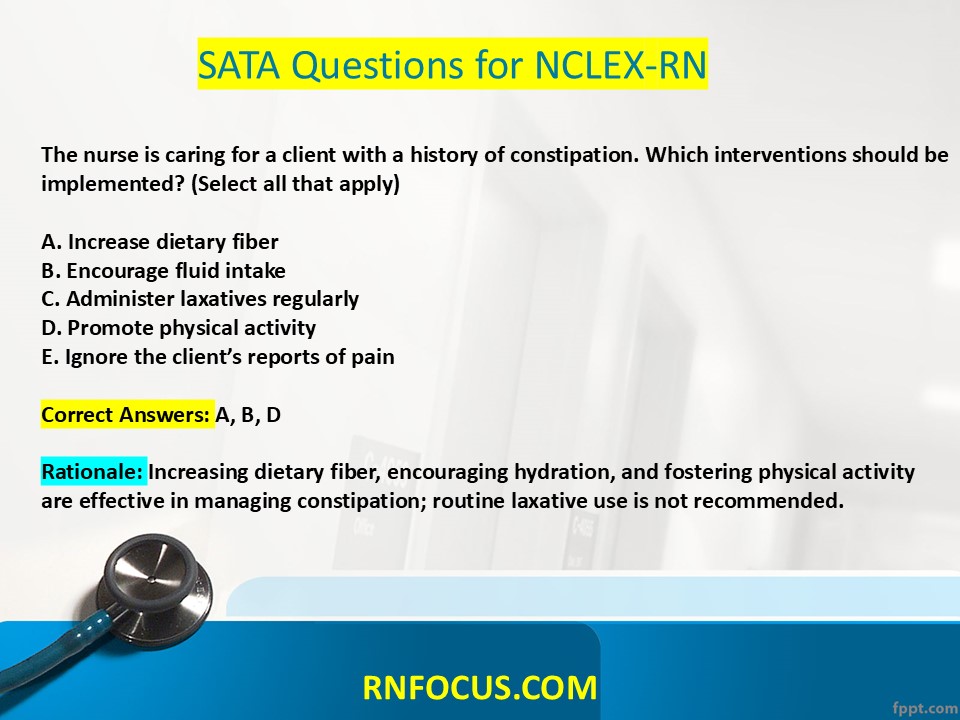
The nurse is caring for a client with a history of constipation. Which interventions should be implemented? (Select all that apply)
A. Increase dietary fiber
B. Encourage fluid intake
C. Administer laxatives regularly
D. Promote physical activity
E. Ignore the client’s reports of pain
Correct Answers: A, B, D
Rationale: Increasing dietary fiber, encouraging hydration, and fostering physical activity are effective in managing constipation; routine laxative use is not recommended.
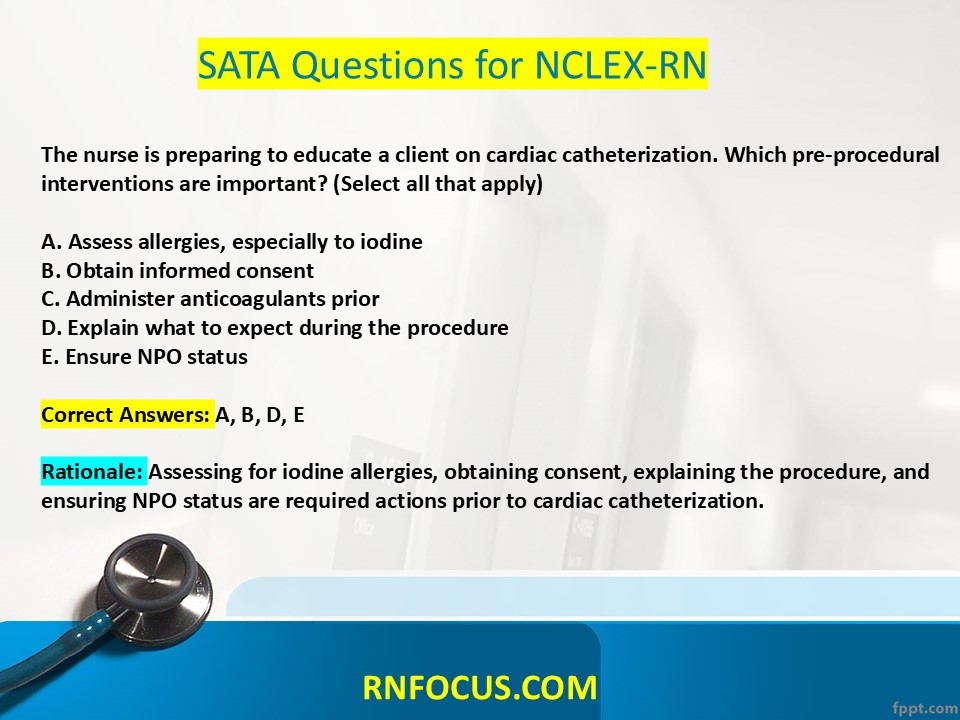
The nurse is preparing to educate a client on cardiac catheterization. Which pre-procedural interventions are important? (Select all that apply)
A. Assess allergies, especially to iodine
B. Obtain informed consent
C. Administer anticoagulants prior
D. Explain what to expect during the procedure
E. Ensure NPO status
Correct Answers: A, B, D, E
Rationale: Assessing for iodine allergies, obtaining consent, explaining the procedure, and ensuring NPO status are required actions prior to cardiac catheterization.
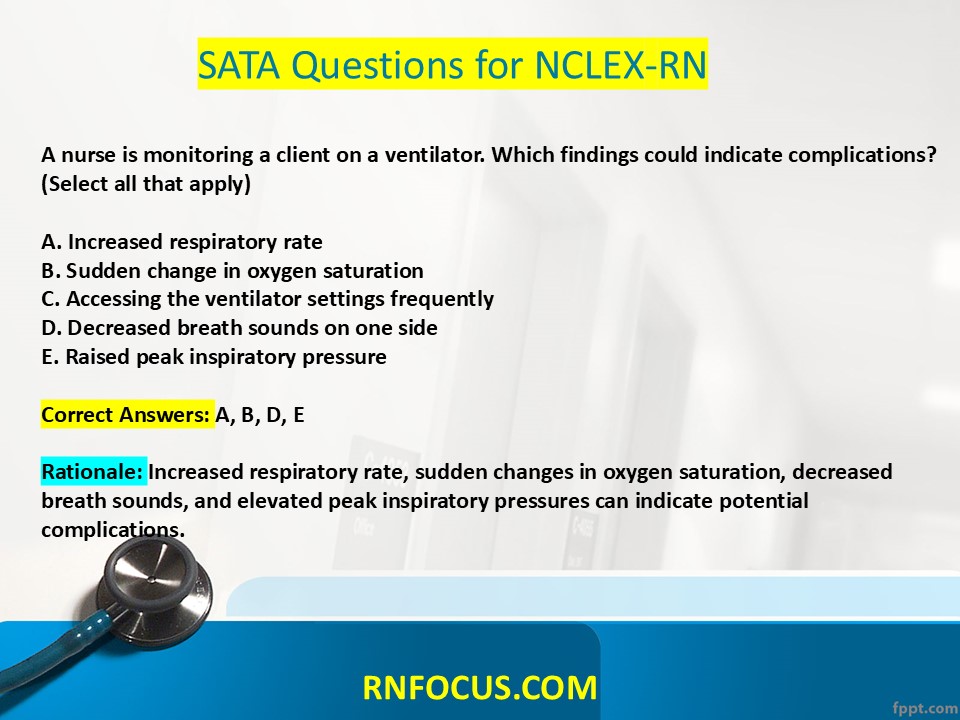
A nurse is monitoring a client on a ventilator. Which findings could indicate complications? (Select all that apply)
A. Increased respiratory rate
B. Sudden change in oxygen saturation
C. Accessing the ventilator settings frequently
D. Decreased breath sounds on one side
E. Raised peak inspiratory pressure
Correct Answers: A, B, D, E
Rationale: Increased respiratory rate, sudden changes in oxygen saturation, decreased breath sounds, and elevated peak inspiratory pressures can indicate potential complications.
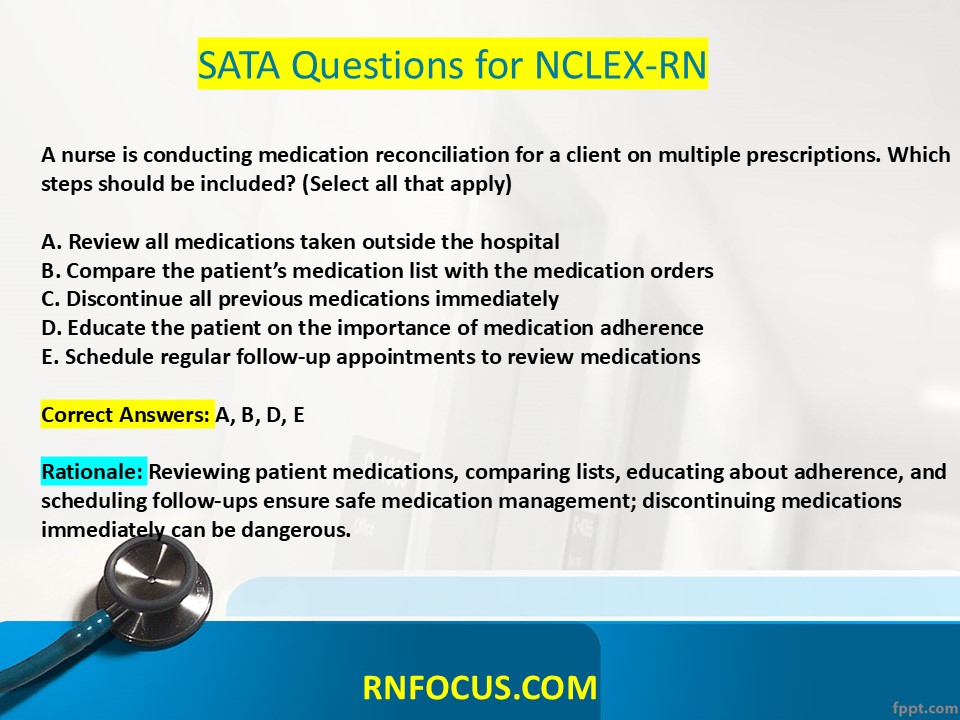
A nurse is conducting medication reconciliation for a client on multiple prescriptions. Which steps should be included? (Select all that apply)
A. Review all medications taken outside the hospital
B. Compare the patient’s medication list with the medication orders
C. Discontinue all previous medications immediately
D. Educate the patient on the importance of medication adherence
E. Schedule regular follow-up appointments to review medications
Correct Answers: A, B, D, E
Rationale: Reviewing patient medications, comparing lists, educating about adherence, and scheduling follow-ups ensure safe medication management; discontinuing medications immediately can be dangerous.
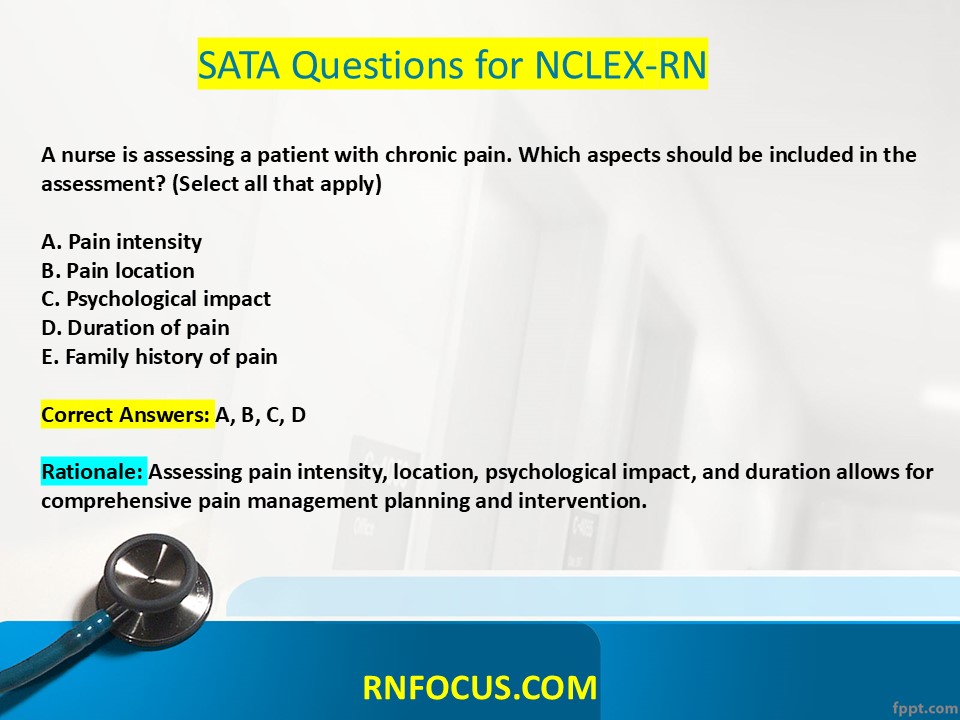
A nurse is assessing a patient with chronic pain. Which aspects should be included in the assessment? (Select all that apply)
A. Pain intensity
B. Pain location
C. Psychological impact
D. Duration of pain
E. Family history of pain
Correct Answers: A, B, C, D
Rationale: Assessing pain intensity, location, psychological impact, and duration allows for comprehensive pain management planning and intervention.
The nurse is providing care for a patient exhibiting signs of delirium. Which interventions should the nurse implement? (Select all that apply)
A. Maintain a calm environment
B. Use restraints for safety
C. Reorient the patient regularly
D. Encourage family involvement
E. Limit stimulation
Correct Answers: A, C, D
Rationale: Maintaining a calm environment, regular reorientation, and involving the family are effective strategies to mitigate confusion and anxiety.
A nurse is preparing to educate a client with hypertension about lifestyle modifications. Which recommendations should the nurse make? (Select all that apply)
A. Engage in regular physical activity
B. Increase sugary food intake
C. Use dietary sodium restrictions
D. Reduce stress levels
E. Avoid regular check-ups
Correct Answers: A, C, D
Rationale: Regular physical activity, reducing sodium intake, and managing stress are integral in hypertension management; increasing sugar intake and avoiding check-ups are poor health strategies.
A nurse is discussing potential side effects with a client newly prescribed a beta-blocker. Which side effects should be included? (Select all that apply)
A. Bradycardia
B. Hypotension
C. Insomnia
D. Fatigue
E. Dry mouth
Correct Answers: A, B, D
Rationale: Side effects can include bradycardia, hypotension, and fatigue; insomnia is less commonly associated.
The nurse is assessing a patient with potential congestive heart failure. Which findings would support this diagnosis? (Select all that apply)
A. Dyspnea on exertion
B. Peripheral edema
C. Crackles upon lung auscultation
D. Normal heart rhythm
E. Elevated jugular venous pressure
Correct Answers: A, B, C, E
Rationale: Dyspnea, peripheral edema, crackles upon auscultation, and elevated JVP are indicators of congestive heart failure.
The nurse is caring for a client undergoing chemotherapy. Which interventions should be prioritized to manage side effects? (Select all that apply)
A. Monitor for signs of infection
B. Provide antiemetics as prescribed
C. Encourage hydration
D. Restrict visitors for safety
E. Encourage a diet high in sugar
Correct Answers: A, B, C
Rationale: Monitoring for infection, administering antiemetics, and encouraging hydration are integral to supportive care during chemotherapy.
A nurse is assessing a patient with pneumonia. Which findings would warrant further investigation? (Select all that apply)
A. Cough with sputum production
B. Dullness upon percussion
C. Increased respiratory rate
D. Clear lung sounds
E. Fever and chills
Correct Answers: A, B, C, E
Rationale: Cough with sputum, dullness on percussion, increased respiratory rate, and fever are findings associated with pneumonia.
The nurse in the emergency department is caring for a client with anaphylaxis. Which interventions should be performed? (Select all that apply)
A. Administer epinephrine
B. Apply oxygen as needed
C. Establish IV access for fluid resuscitation
D. Document the patient’s medical history
E. Place the patient in a supine position
Correct Answers: A, B, C
Rationale: Administering epinephrine, applying oxygen, and establishing IV access for fluids are immediate interventions in anaphylaxis.
A nurse is assessing a patient with seizures. What ambulatory teaching should be provided? (Select all that apply)
A. Take medications as prescribed
B. Avoid alcohol consumption
C. Chart all seizure occurrences
D. Use safety precautions during activities
E. Maintain a high-protein diet
Correct Answers: A, B, C, D
Rationale: Adherence to medications, avoiding alcohol, charting seizures, and safety precautions are crucial for managing seizure disorders.
A nurse is reviewing discharge instructions for a client with a new colostomy. Which topics should be included? (Select all that apply)
A. Stoma care and hygiene
B. Dietary restrictions
C. Ostomy bag changes
D. Signs of complications
E. Importance of routine appointments
Correct Answers: A, B, C, D, E
Rationale: Stoma care, dietary considerations, bag changes, signs of complications, and follow-ups are critical teaching points for colostomy management.
A nurse is assessing a client with chronic kidney disease about medication management. Which statements indicate the need for further teaching? (Select all that apply)
A. “I can take over-the-counter NSAIDs as needed.”
B. “I’ll regularly monitor my blood pressure.”
C. “I’ll limit my fluid intake as prescribed.”
D. “I can increase my potassium intake.”
E. “I must take all prescribed medications.”
Correct Answers: A, D
Rationale: Over-the-counter NSAIDs and increased potassium intake can exacerbate kidney disease; adherence to prescribed medications is crucial for management.
A nurse is assessing a patient with atrial fibrillation. Which findings should the nurse monitor closely? (Select all that apply)
A. Irregular heart rate
B. Shortness of breath
C. Chest discomfort
D. Lower extremity edema
E. Elevated blood glucose
Correct Answers: A, B, C, D
Rationale: Monitoring irregular heart rate, shortness of breath, chest discomfort, and lower extremity edema is crucial in managing patients with atrial fibrillation.
The nurse is forming a care plan for a patient with chronic pain. Which interventions will the nurse include? (Select all that apply)
A. Employing both pharmacologic and non-pharmacologic therapies
B. Encouraging regular physical activity
C. Focusing on the psychological aspects of pain
D. Scheduling frequent pain assessments
E. Educating about complementary treatments
Correct Answers: A, B, C, D, E
Rationale: Integrating pharmacologic and non-pharmacologic therapies, promoting physical activity, and educating patients about complementary treatments can effectively manage chronic pain.
The nurse is assessing a patient with diabetes for signs of hyperglycemia. Which findings might the nurse observe? (Select all that apply)
A. Polyuria
B. Polydipsia
C. Fatigue
D. Blurred vision
E. Weight loss
Correct Answers: A, B, C, D
Rationale: Signs of hyperglycemia include polyuria, polydipsia, fatigue, and blurred vision; weight loss might occur, but it is not a reliable indicator alone.
A nurse is monitoring a patient receiving total parenteral nutrition (TPN). Which assessments should be prioritized? (Select all that apply)
A. Daily weight
B. Blood glucose levels
C. IV site integrity
D. TPN infusion rate
E. Electrolyte levels
Correct Answers: A, B, C, D
Rationale: Daily weight, blood glucose levels, IV site integrity, and TPN infusion rate are critical assessments during TPN administration.
A nurse is educating a client about infection prevention while on immunosuppressive therapy. Which instructions are essential? (Select all that apply)
A. Avoid crowds and sick individuals
B. Maintain good personal hygiene
C. Take vaccinations as directed
D. Stop taking immunosuppressants if symptoms occur
E. Report signs of infection immediately
Correct Answers: A, B, E
Rationale: To reduce infection risk, patients should avoid crowded areas, maintain hygiene, and report any signs of infection immediately; stopping medications without consulting can be dangerous.
The nurse is assessing a patient after a myocardial infarction. Which assessments are crucial during the recovery phase? (Select all that apply)
A. Cardiac rhythm via telemetry
B. Neurological status
C. Pain assessment
D. Nutritional intake
E. Mobility status
Correct Answers: A, B, C, D
Rationale: Monitoring cardiac rhythm, neurological status, pain, and nutritional intake after myocardial infarction is critical for effective recovery.
A nurse is caring for a young adult with depression. Which interventions should the nurse include in the care plan? (Select all that apply)
A. Encourage participation in support groups
B. Promote regular exercise
C. Limit social interactions
D. Monitor for suicidal ideation
E. Normalize the patient’s feelings and experiences
Correct Answers: A, B, D
Rationale: Encouraging participation in support groups, promoting exercise, and monitoring for suicidal ideation help address the complexities of depression.
The nurse is teaching a client with chronic liver disease about dietary management. Which considerations should be discussed? (Select all that apply)
A. Avoid high-protein diets
B. Limit alcohol intake
C. Increase sodium consumption
D. Consume small, frequent meals
E. Ensure adequate hydration
Correct Answers: A, B, D, E
Rationale: Avoiding high-protein diets, limiting alcohol intake, consuming small meals, and ensuring hydration are all essential dietary strategies for managing chronic liver disease.
The nurse is monitoring a client receiving chemotherapy. Which assessments would indicate potential complications? (Select all that apply)
A. Mouth sores
B. Frequent infections
C. Nausea and vomiting
D. Hair loss
E. Improved energy levels
Correct Answers: A, B, C, D
Rationale: Mouth sores, infections, nausea, and hair loss commonly occur with chemotherapy and indicate complications or side effects.
A nurse is caring for a patient with pancreatitis. Which nursing actions are appropriate? (Select all that apply)
A. Withhold oral intake
B. Monitor serum amylase and lipase levels
C. Position the patient in a supine position
D. Assess for signs of hemorrhage
E. Administer prescribed analgesics
Correct Answers: A, B, D, E
Rationale: Withholding oral intake, monitoring metabolic markers, assessing for complications, and ensuring effective analgesia are vital in managing pancreatitis.
A nurse is educating a client with rheumatoid arthritis about self-management. Which strategies should be included? (Select all that apply)
A. Use of assistive devices
B. Engage in high-impact exercises
C. Implementing heat and cold therapy
D. Balancing rest and activity
E. Maintaining a healthy weight
Correct Answers: A, C, D, E
Rationale: Using assistive devices, implementing heat and cold therapy, balancing rest and activity, and maintaining a healthy weight are effective strategies for managing rheumatoid arthritis.
A nurse is preparing to administer a blood transfusion. Which steps should be taken prior to administration? (Select all that apply)
A. Verify blood type and donor information
B. Assess baseline vital signs
C. Administer premedications as ordered
D. Obtain a second nurse’s verification
E. Start the transfusion at a high rate
Correct Answers: A, B, D
Rationale: Verifying blood type and donor information, assessing vital signs, and obtaining a second verification are essential steps before a transfusion; starting the transfusion at a high rate poses risk for reactions.
A nurse is working with a client diagnosed with bipolar disorder. Which interventions promote stabilization during manic episodes? (Select all that apply)
A. Maintain a structured environment
B. Encourage high stimulation activities
C. Monitor sleep patterns
D. Provide clear, concise communication
E. Reinforce medication adherence
Correct Answers: A, C, D, E
Rationale: Maintaining structure, monitoring sleep, providing clear communication, and reinforcing medication adherence are effective strategies during manic episodes.
The nurse is assessing a preschool-age child. Which developmental milestones should be expected? (Select all that apply)
A. Ability to ride a tricycle
B. Ability to dress independently
C. Vocabulary of 200-300 words
D. Ability to hop on one foot
E. Ability to tie shoelaces
Correct Answers: A, B, C, D
Rationale: Riding a tricycle, dressing independently, having a vocabulary of 200-300 words, and the ability to hop on one foot are developmental milestones for preschoolers.
A nurse is caring for a client after a hip replacement. Which postoperative interventions are critical? (Select all that apply)
A. Monitor vital signs closely
B. Encourage deep breathing exercises
C. Restrict fluid intake
D. Promote mobility as tolerated
E. Educate on signs of infection
Correct Answers: A, B, D, E
Rationale: Monitoring vital signs, encouraging deep breathing, promoting mobility, and educating on infection signs are critical components of postoperative care.
This format provides a thorough understanding of each question, the correct answers, and the rationale behind them. Good luck with your studies!