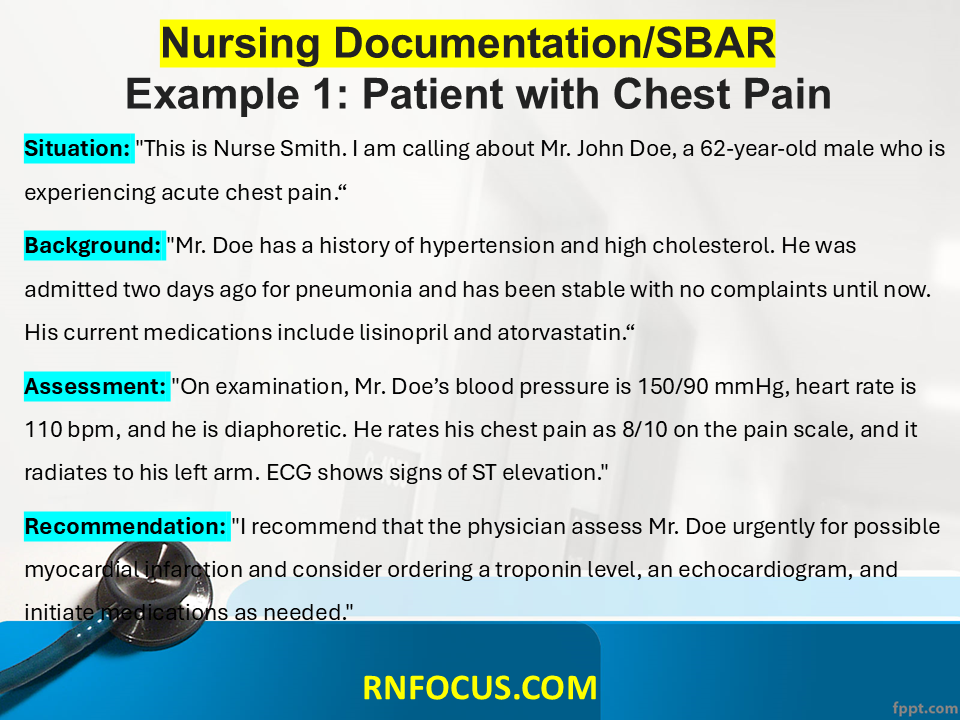
Example 1: Patient with Chest Pain
Situation:
- “This is Nurse Smith. I am calling about Mr. John Doe, a 62-year-old male who is experiencing acute chest pain.”
Background:
- “Mr. Doe has a history of hypertension and high cholesterol. He was admitted two days ago for pneumonia and has been stable with no complaints until now. His current medications include lisinopril and atorvastatin.”
Assessment:
- “On examination, Mr. Doe’s blood pressure is 150/90 mmHg, heart rate is 110 bpm, and he is diaphoretic. He rates his chest pain as 8/10 on the pain scale, and it radiates to his left arm. ECG shows signs of ST elevation.”
Recommendation:
- “I recommend that the physician assess Mr. Doe urgently for possible myocardial infarction and consider ordering a troponin level, an echocardiogram, and initiate medications as needed.”
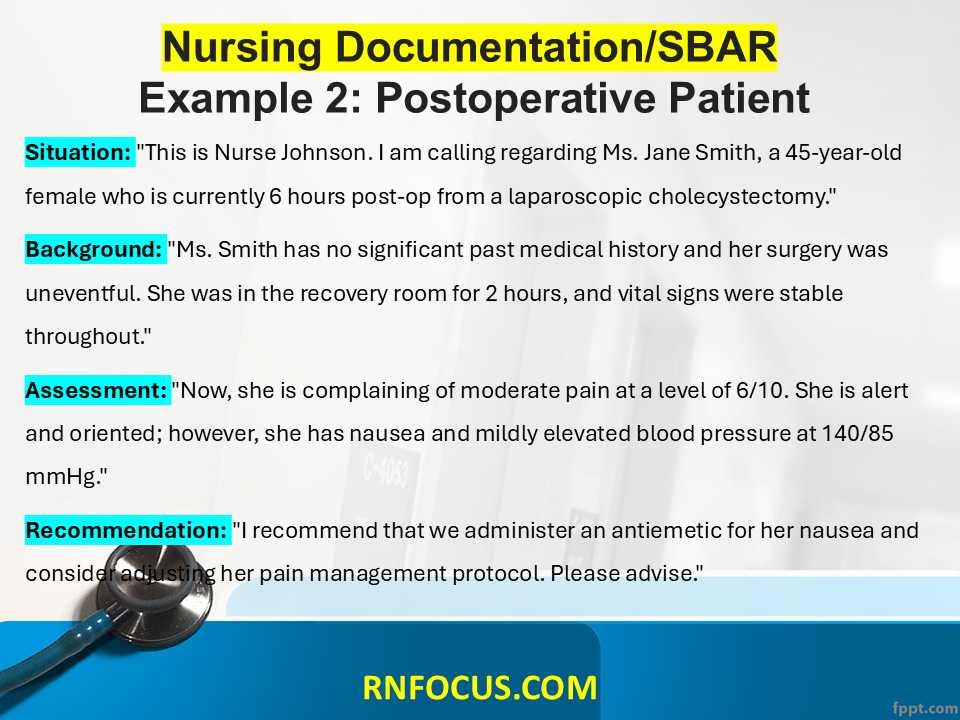
Example 2: Postoperative Patient
Situation:
- “This is Nurse Johnson. I am calling regarding Ms. Jane Smith, a 45-year-old female who is currently 6 hours post-op from a laparoscopic cholecystectomy.”
Background:
- “Ms. Smith has no significant past medical history and her surgery was uneventful. She was in the recovery room for 2 hours, and vital signs were stable throughout.”
Assessment:
- “Now, she is complaining of moderate pain at a level of 6/10. She is alert and oriented; however, she has nausea and mildly elevated blood pressure at 140/85 mmHg.”
Recommendation:
- “I recommend that we administer an antiemetic for her nausea and consider adjusting her pain management protocol. Please advise.”
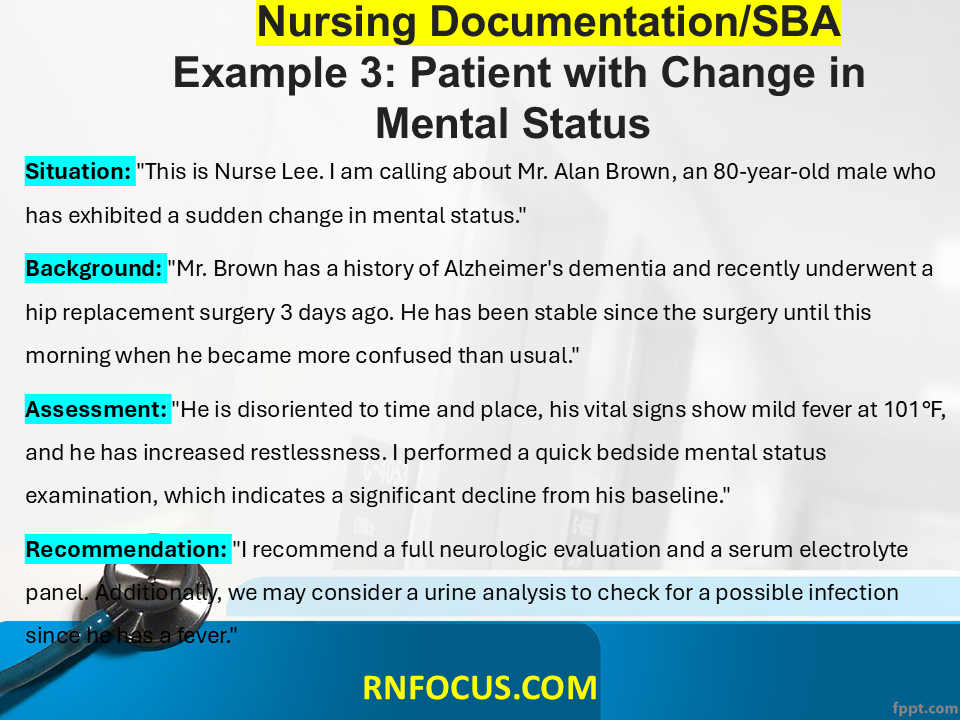
Example 3: Patient with Change in Mental Status
Situation:
- “This is Nurse Lee. I am calling about Mr. Alan Brown, an 80-year-old male who has exhibited a sudden change in mental status.”
Background:
- “Mr. Brown has a history of Alzheimer’s dementia and recently underwent a hip replacement surgery 3 days ago. He has been stable since the surgery until this morning when he became more confused than usual.”
Assessment:
- “He is disoriented to time and place, his vital signs show mild fever at 101°F, and he has increased restlessness. I performed a quick bedside mental status examination, which indicates a significant decline from his baseline.”
Recommendation:
- “I recommend a full neurologic evaluation and a serum electrolyte panel. Additionally, we may consider a urine analysis to check for a possible infection since he has a fever.”
Example 4: Patient with Respiratory Distress
Situation:
- “This is Nurse Garcia. I am calling about Mrs. Emily White, a 74-year-old female who is experiencing significant respiratory distress.”
Background:
- “Mrs. White has a history of COPD and was admitted for exacerbation of her condition. She has been on oxygen therapy since admission with a target saturation of 92%.”
Assessment:
- “Currently, her SpO2 is 85% on 6 L of nasal cannula, and she is using accessory muscles to breathe. Auscultation reveals wheezing and diminished breath sounds bilaterally.”
Recommendation:
- “I recommend an increase in oxygen flow to 10 L and consider administering a nebulized bronchodilator. Please evaluate her for potential admission to the ICU.”
Example 5: Patient with Elevated Blood Sugar
Situation:
- “This is Nurse Thompson. I’m calling about Mr. Henry Lee, a 55-year-old male, who has an elevated glucose level.”
Background:
- “Mr. Lee has a history of type 2 diabetes but has been non-compliant with his medication regimen. He was admitted for a diabetic foot ulcer and has been receiving insulin.”
Assessment:
- “His blood sugar level is currently 350 mg/dL. He is alert but appears anxious. He reports not having taken his insulin for the past two days due to nausea.”
Recommendation:
- “I recommend we adjust his insulin regimen and provide patient education on managing his diabetes. Please consider an endocrinology consult for further management.”
Example 6: Patient with Urinary Complications
Situation:
- “This is Nurse Patel. I am calling about Ms. Sara Johnson, a 32-year-old female with new-onset urinary retention.”
Background:
- “Ms. Johnson has a history of multiple sclerosis. She has been admitted for relapse and has been unable to void for the past 10 hours.”
Assessment:
- “The bladder scan shows 800 mL of retained urine, and she is complaining of lower abdominal discomfort. She is afebrile and vital signs are stable.”
Recommendation:
- “I recommend a trial of intermittent catheterization to relieve her urinary retention and consult her neurologist for a potential adjustment in her management plan.”
Example 7: Patient with Fever after Surgery
Situation:
- “This is Nurse Robinson. I am calling about Mr. Tom Smith, a 68-year-old male, who has developed a fever post-surgery.”
Background:
- “Mr. Smith underwent a total knee replacement 24 hours ago. He has no significant history of infection prior to surgery and has been recovering well.”
Assessment:
- “His temperature is 102°F, and he appears flushed and slightly agitated. Surgical site inspection shows no signs of redness or drainage.”
Recommendation:
- “I recommend blood cultures be drawn and initiate a broad-spectrum antibiotic regimen while we await results. Please evaluate him for possible sources of infection.”
Example 8: Patient with Acute Abdomen Pain
Situation:
- “This is Nurse Kim. I am calling about Ms. Sarah Thompson, a 29-year-old female presenting with acute abdominal pain.”
Background:
- “Ms. Thompson has no previous abdominal surgeries and has been healthy. She was admitted with abdominal pain that began suddenly in the lower right quadrant.”
Assessment:
- “She rates her pain as 9/10, is guarding her abdomen, and has tenderness in the right lower quadrant. No bowel sounds are heard upon auscultation.”
Recommendation:
- “I recommend that the physician assess her for possible appendicitis and order an abdominal ultrasound. Pain management should also be initiated.”
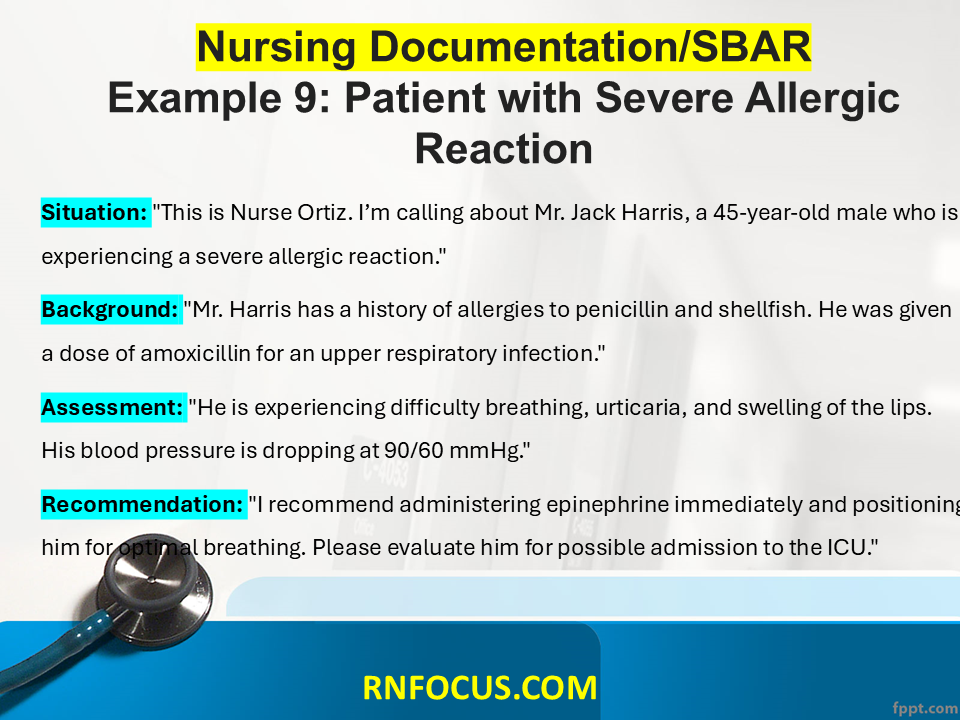
Example 9: Patient with Severe Allergic Reaction
Situation:
- “This is Nurse Ortiz. I’m calling about Mr. Jack Harris, a 45-year-old male who is experiencing a severe allergic reaction.”
Background:
- “Mr. Harris has a history of allergies to penicillin and shellfish. He was given a dose of amoxicillin for an upper respiratory infection.”
Assessment:
- “He is experiencing difficulty breathing, urticaria, and swelling of the lips. His blood pressure is dropping at 90/60 mmHg.”
Recommendation:
- “I recommend administering epinephrine immediately and positioning him for optimal breathing. Please evaluate him for possible admission to the ICU.”
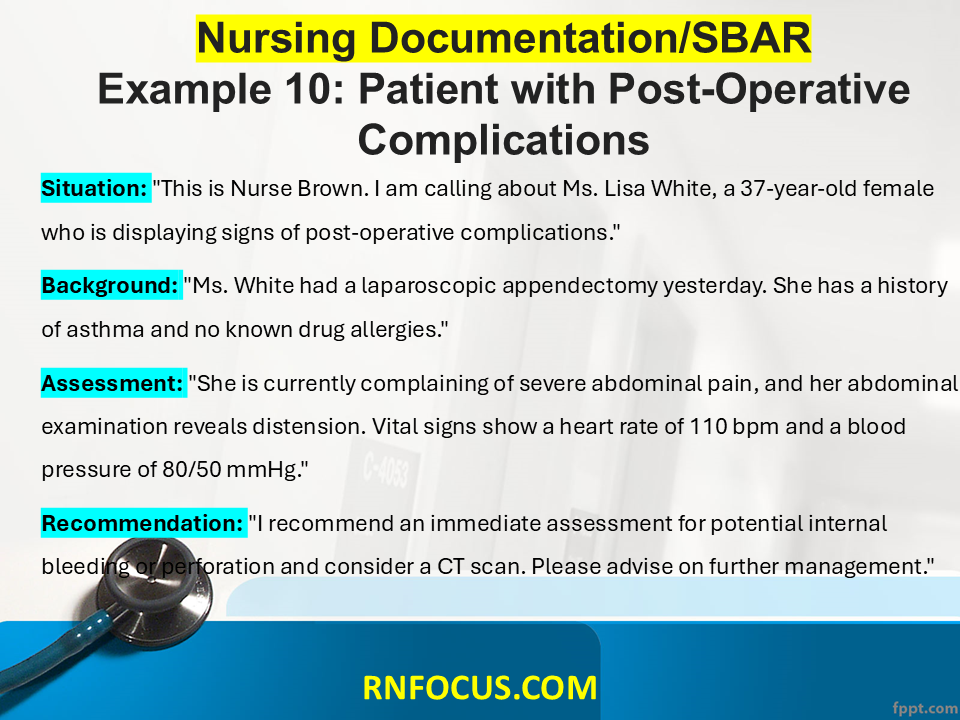
Example 10: Patient with Post-Operative Complications
Situation:
- “This is Nurse Brown. I am calling about Ms. Lisa White, a 37-year-old female who is displaying signs of post-operative complications.”
Background:
- “Ms. White had a laparoscopic appendectomy yesterday. She has a history of asthma and no known drug allergies.”
Assessment:
- “She is currently complaining of severe abdominal pain, and her abdominal examination reveals distension. Vital signs show a heart rate of 110 bpm and a blood pressure of 80/50 mmHg.”
Recommendation:
- “I recommend an immediate assessment for potential internal bleeding or perforation, and consider a CT scan. Please advise on further management.”



Magnificent web site. Lots of helpful information here.
I am sending it to some friends ans additionally sharing in delicious.
And obviously, thanks to your effort!
I like this post, enjoyed this one thanks for posting.